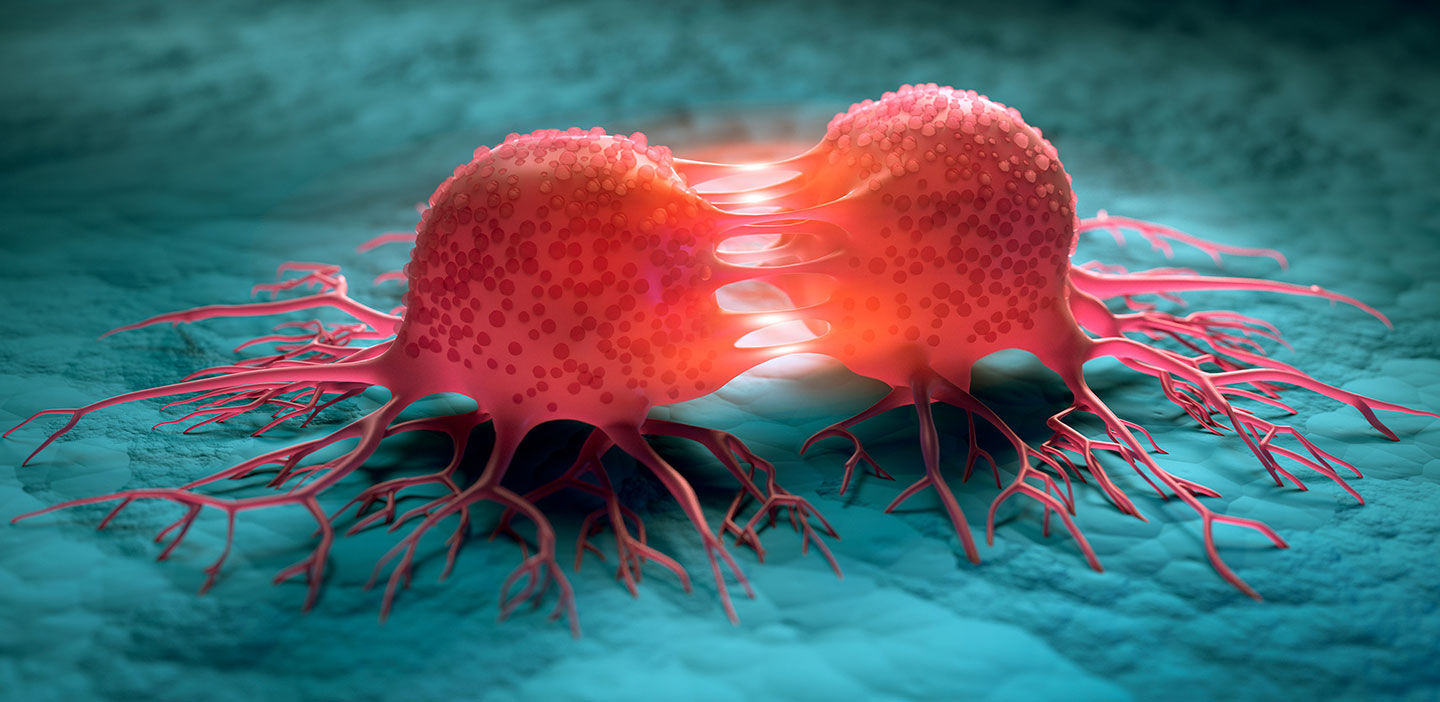
How does a normal cell transform into a cancerous cell? The transformation is complex. The transition takes place over time with cells manifesting several signature phenotypic and genotypic alterations. In a normal cell, cell division is facilitated by several interacting genes through defined signal transduction pathways. In addition, mechanisms that control or regulate cell division also exist. The intricately maintained balance between cell proliferation and suppression sustain the normal functioning of cells.
Cancer cells, however, are typified by an imbalance between these two functions. In addition, over the course of cancer development, several characteristics are acquired by cancer cells. The typically understood characteristics, classified as major hallmarks of cancer, are: sustained proliferation, evading growth suppressors, activating invasion and metastasis, enabling immortality, inducing angiogenesis, resisting cell death, reprogramming of energy metabolism and evading destruction by the immune system.1 Such a display of complex characteristics involves accumulation of several alterations in genes (mutations). Understanding these mutations provide opportunities to develop novel ways to tackle the disease.